Exeter MR Research Centre
Clinical Cardiac Group
Collaborators
 Dr David Ripley
Dr David Ripley
 Linda Haynes
Linda Haynes
 Andy Pitt
Andy Pitt
 Danielle Cox
Danielle Cox
 Dr Nick Bellinger
Dr Nick Bellinger
1- SUMMIT
| Summary |
The study aims to perform a comprehensive examination of cardiac structure and function in individuals with and without type 2 diabetes, and, with and without known cardiovascular disease at baseline, and to follow-up and repeat these assessments after 3 to 4 years. The specific objectives of this investigation are:
1) to compare the prevalence and severity of myocardial dysfunction, coronary and cardiac microvascular disease between diabetic and non diabetic subjects.
2) to establish if cardiac functional abnormalities are associated with systemic microvascular dysfunction or are unique to the heart.
3) to determine whether the presence of cardiovascular disease has an additive effect on cardiac dysfunction in individuals with type.
2 diabetes compared to individuals without diabetes.
4) to explore how cardiac dysfunction changes as diabetes and cardiovascular disease progress with time.
5) to examine whether a cardiac functional abnormality has the potential to predict future progression of cardiovascular disease.
6) to investigate links between hepatic and intramyocardial fat with vascular function.
|
2- Syndrome X
| Summary |
Classical cardiac syndrome X is defined as typical angina of effort, ST depression at exercise ECG testing and normal coronary arteries at invasive coronary angiography. This classical definition requires the presence of a positive exercise tolerance test- which has a poor accuracy even in the presence of marked epicardial coronary stenosis. A new definition encompassing the typical symptoms of angina together with normal coronary arteries but using other forms of stress testing, rather than the exercise ECG, has been proposed.
Some now feel that the classical diagnosis should be abandoned for a more homogenous term that encompasses any pain which can reasonably be attributed to cardiac microvascular dysfunction rather than the heterogeneous syndrome of chest pain with normal or un-obstructed coronary arteries.
The matter is confused by the varying diagnostic criteria in the literature- some authors stressing that the invasive coronary angiogram should be completely normal while others accept non-flow limiting stenosis. 10-30% of patients referred for coronary angiography will have normal or near normal coronary arteries.
Blood flow within the epicardial conduit vessels is dictated by the vascular tone within the microcirculation – arterioles, capillaries and venules of less than 100 microns in diameter. Ischaemia in the presence of normal or near normal epicardial coronary vessels is thought to be due to microvascular dysfunction. Previous publications have used invasive angiography as a means to assess the “normalility” of the epicardial coronary circulation. However an invasive coronary angiogram can not rule out the presence of expansive remodelling-atheroma affecting the coronary artery but not impinging on the vessel lumen. The presence of non-stenotic coronary atheroma can result in a significant reduction in the pressure along a diffusely stenosed coronary vessel and therefore produce a perfusion defect which is not caused by microcirculatory dysfunction. 60-70% of patients with syndrome X will have atheromatous change or marked intimal thickening which have an effect on any testing of the microcirculation and endothelial function.
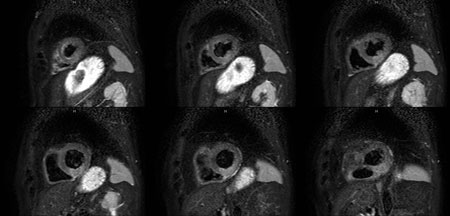
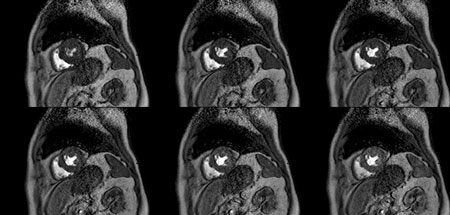
Cardiac stress magnetic resonance imaging is in routine use for the diagnosis of ischaemic heart disease and is used to track the first pass perfusion of gadolinium as it enters the myocardium; this is preformed at stress (with adenosine, dipyridamole or dobutamine) and at rest and the two images compared. As the contrast agent enters the myocardium the signal intensity can be plotted against time to produce a signal intensity curve. The signal intensity (SI) gradient of the myocardium is divided by the signal intensity gradient from the left ventricular blood pool to correct for changes in loading conditions due to the effect of the stressor agent giving the myocardium perfusion index (MPI). The ratio of the MPI between stress and rest imaging is the myocardial perfusion reserve index (MPRI). Quantitative assessment of myocardial perfusion (MPRI) correlates with endothelial dependant and independent vascular function which are reduced in cardiac syndrome X and other conditions known to effect the microcirculation. MRI myocardial perfusion defects are present in patients with endothelial dysfunction of the cardiac epicardial vessels and microcirculation.
Controversy exists as to the nature of changes seen at MRI perfusion in cardiac syndrome X. Groups incorporating an abnormal ETT in the diagnostic criteria have demonstrated sub-endocardial perfusion defects at stress MRI; however other studies have failed to demonstrated a sub-endocardial defect . This difference may be due to the differing patient cohorts and definition of syndrome X used by the researchers.
We propose to study a symptomatic population who have no or very little coronary atheroma at cardiac CT and assess their cardiac and peripheral microcirculation. We will also use a quantitative assessment of the myocardial perfusion rather than qualitative used in previous studies.
|
3- MVO
| Summary |
Acute Myocardial Infarction (MI) is the biggest cause of Death in the UK. Current optimum management includes emergent (primary) coronary intervention (angioplasty/coronary stent insertion) for all patients presenting within 6 hours of acute MI. After primary coronary intervention (PCI), despite visibly restored flow in the coronary arteries, cardiac magnetic resonance (CMR) imaging has demonstrated areas of hypo or no-perfusion of the heart muscle (myocardium) supplied by these vessels. This phenomenon of ‘no-reflow’ or microvascular (small vessel) obstruction (MVO) is known to complicate up to 70% of emergent angioplasties. The presence of MVO predisposes the patient to post infarction heart failure, additional MI and cardiac death.
We aim to determine the incidence of MVO on CMR following acute MI/primary PCI in the presence and absence of systemic microvascular dysfunction (determined on the basis of non invasive techniques and blood and urine biomarkers) and compare the two. Higher incidence of MVO in the presence of systemic microvascular impairment would indicate a role of microvascular disease in the pathophysiology of MVO.
We will also quantify myocardial recovery, LV remodelling and infarct size using CMR in the presence and absence of systemic microvascular dysfunction (determined on the basis of non invasive techniques and blood and urine biomarkers) and compare the two. Impaired myocardial recovery, increased LV remodelling or increased infarct size in the presence of systemic microvascular impairment would be consistent with a negative prognostic effect of intra-myocardial microvascular dysfunction not purely as a result of infarction but as part of systemic microvascular impairment.
|
4- Constriction
| Summary |
Coronary artery bypass grafting (CABG) is one of the most common cardiac operations performed world wide. One rare but serious complication in the years following CABG is the development of pericardial constriction. The pericardium is a fibrous sack within the chest that the heart sits in. It is normally an elastic pliable structure that moves with the beating of the heart. One of the late complications of by-pass surgery is thickening of the pericardium resulting in pericardial constriction. Differentiating pericardial constriction from heart failure due to left ventricular dysfunction is of vital importance as there are marked differences in the treatments for these two conditions. There are certain characteristics of pericardial constriction which can be identified on Cardiac MRI scanning. These have been studied in a population known or suspected of having pericardial constriction because of their clinical presentation. However it is not clear whether CMR features of constriction are common following cardiac surgery, whether they are present in the weeks following surgery and resolve, or persist as part of a normal feature on CMR scanning. We aim to use the high spatial and temporal resolution imaging offered by cardiac MRI to investigate the normal changes undergone by the pericardium just prior, 6 weeks and then 6 months following bypass grafting to identify the normal features of the pericardium following CABG. This research will give clinicians a base line MRI assessment of the heart to help interpret cardiac MRI scans in patients referred for the investigation of suspected pericardial constriction following CABG.
The MRI protocol will include-
- Scout scans of the chest and abdomen.
- Axial scans of the chest and abdomen.
- Short and long axis cine images of the Left ventricle for function.
- T1 and T2 weighted images of the heart and pericardium.
- Free breathing cine images of the left ventricle.
- Velocity encoded images of the Aorta for LV stroke volume.
|